Introduction: The Critical Role of Compliance in Medical Billing
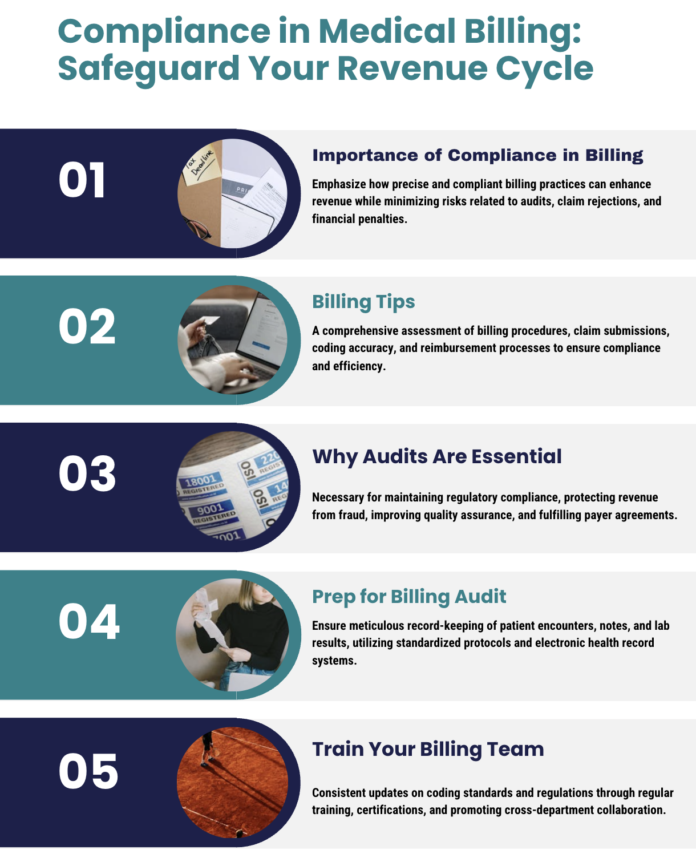
Medical billing is the financial lifeline of any healthcare practice. Ensuring that your billing processes are accurate and compliant not only maximizes revenue but also minimizes the risk of audits, claim denials, and regulatory penalties. With the increasing scrutiny of healthcare reimbursements and constant updates in payer guidelines, medical practices must be proactive in managing their billing systems.
Medical billing audits are a routine part of the healthcare landscape, designed to verify the accuracy and integrity of billing practices. However, the process can be daunting. When audits are handled efficiently, they serve as an opportunity to identify process gaps, improve internal workflows, and ultimately enhance cash flow. Conversely, poorly managed audits can result in lost revenue, fines, and reputational damage.
This comprehensive guide explores how to handle medical billing audits effectively and stay compliant with ever-evolving healthcare regulations. Whether you’re a small private practice or a large multi-specialty clinic, the following expert strategies will help you prepare for audits, manage them efficiently, and ensure continuous compliance to protect your revenue cycle.
1. Understanding Medical Billing Audits
1.1 What Is a Medical Billing Audit?
A medical billing audit is a systematic review of your practice’s billing processes, claims submissions, coding accuracy, and reimbursement procedures. The primary purpose of an audit is to ensure that the services billed are accurately documented, compliant with federal and state regulations, and that reimbursements are appropriate for the care provided. Audits can be initiated by insurance payers, government agencies (such as Medicare and Medicaid), or conducted internally as part of quality assurance measures.
1.2 Why Do Audits Happen?
Audits occur for several reasons:
- Regulatory Compliance: Government agencies and insurers conduct audits to ensure that practices adhere to billing guidelines and regulatory requirements.
- Revenue Protection: To prevent fraud, waste, and abuse, audits help identify discrepancies between the services provided and the amounts billed.
- Quality Assurance: Internal audits are used to assess the effectiveness of billing processes and identify areas for improvement.
- Payer Agreements: Some insurance contracts require periodic audits to verify that claims are processed in accordance with agreed-upon standards.
Understanding the reasons behind audits is the first step in developing a proactive strategy to handle them, ensuring that your practice remains compliant and financially healthy.
2. Preparing for a Medical Billing Audit
2.1 Establish Robust Documentation Practices
Accurate documentation is the cornerstone of successful medical billing. To prepare for an audit:
- Maintain Complete Records: Ensure that all patient encounters, services rendered, and supporting documents (such as physician notes, diagnostic reports, and lab results) are complete and up-to-date.
- Implement a Standardized Process: Develop and enforce standardized procedures for data entry, coding, and charge capture. This minimizes errors and ensures consistency across your practice.
- Use Electronic Health Records (EHR) Effectively: EHR systems should integrate seamlessly with your billing software to capture all necessary information automatically.
2.2 Train Your Billing and Coding Staff
Well-trained staff can make a significant difference in reducing errors:
- Ongoing Training: Regularly update your staff on the latest coding guidelines, regulatory changes, and best practices in medical billing.
- Certifications and Continuing Education: Encourage billing and coding professionals to obtain certifications (e.g., CPC, CCS) and participate in continuing education programs.
- Cross-Departmental Collaboration: Facilitate communication between clinical and billing departments to ensure that documentation accurately reflects the services provided.
2.3 Conduct Internal Audits Regularly
Before an external audit, perform regular internal reviews:
- Monthly or Quarterly Audits: Schedule routine audits to identify discrepancies, underbilling, or overbilling issues early.
- Utilize Audit Software: Leverage audit management tools and AI-driven analytics to monitor claim submission accuracy and identify patterns that may lead to denials.
- Create Audit Checklists: Develop comprehensive checklists covering every stage of the billing process, from patient registration to payment posting.
2.4 Leverage Technology and Automation
Modern RCM (Revenue Cycle Management) software can streamline the audit preparation process:
- Automated Claim Scrubbing: Use software that automatically reviews claims for errors before submission.
- Real-Time Eligibility Verification: Ensure that patient insurance details are verified in real time to prevent claim rejections.
- Integrated Analytics: Utilize dashboards and reporting tools that provide real-time insights into billing performance and potential red flags.
3. Best Practices During a Medical Billing Audit
3.1 Be Proactive and Transparent
When an audit begins, a proactive approach can alleviate stress:
- Designate an Audit Coordinator: Assign a dedicated team member to serve as the point of contact with auditors. This person should be well-versed in the practice’s billing processes.
- Maintain Open Communication: Ensure that auditors have access to all requested documentation and are kept informed about any internal corrective actions being taken.
- Document Your Processes: Provide clear, written procedures and policies that demonstrate your commitment to compliance and billing accuracy.
3.2 Respond Promptly to Auditor Requests
Audits can uncover issues that require immediate attention:
- Timely Responses: Address auditor inquiries and requests for additional documentation as quickly as possible.
- Accurate Data Submission: Double-check all information provided to ensure its accuracy, as mistakes can lead to further delays or penalties.
- Corrective Action Plans: If discrepancies are found, work collaboratively with auditors to develop and implement corrective measures.
3.3 Use the Audit as a Learning Opportunity
Audits are not solely punitive—they can be a valuable tool for improvement:
- Identify Systemic Issues: Look for patterns in the audit findings that indicate broader process issues.
- Implement Training Programs: Use audit results to develop targeted training sessions for billing and coding staff.
- Update Policies and Procedures: Revise your internal processes based on auditor feedback to prevent similar issues in the future.
4. Post-Audit Actions and Continuous Compliance
4.1 Analyze Audit Findings Thoroughly
After an audit, take the time to analyze the results:
- Review Denial Codes and Error Patterns: Identify the most common reasons for claim denials or discrepancies.
- Assess Financial Impact: Calculate how much revenue was lost due to billing errors and determine the overall financial impact on your practice.
- Document Findings: Create a detailed report that outlines audit findings, corrective actions taken, and areas for future improvement.
4.2 Implement a Corrective Action Plan
Based on your audit analysis, develop a plan to address the issues:
- Set Clear Objectives: Define specific, measurable goals to improve billing accuracy and compliance.
- Assign Responsibilities: Ensure that each area of deficiency is addressed by a designated team member.
- Timeline for Improvement: Establish a realistic timeline for implementing changes and re-auditing to gauge progress.
4.3 Continuous Training and Process Improvement
Compliance is an ongoing effort:
- Regular Refresher Courses: Schedule periodic training sessions for all billing and coding staff.
- Monitor Regulatory Changes: Stay updated on new billing guidelines, coding updates, and compliance regulations.
- Leverage Feedback: Encourage staff to provide feedback on billing processes and use this information to make continuous improvements.
- Periodic Internal Audits: Keep the momentum by conducting regular internal audits, ensuring that improvements are maintained over time.
5. Common Pitfalls and How to Avoid Them
5.1 Incomplete Documentation
Pitfall: Inadequate documentation can lead to claim denials and non-compliance issues. Solution: Ensure that every patient encounter is documented in detail, and that documentation is reviewed regularly by both clinical and billing teams.
5.2 Lack of Staff Training
Pitfall: Inexperienced or inadequately trained staff can contribute to coding errors and billing mistakes. Solution: Invest in ongoing training, certifications, and regular audits to keep staff updated on best practices and regulatory changes.
5.3 Overreliance on Manual Processes
Pitfall: Manual billing processes are prone to human error, which can lead to both underbilling and overbilling. Solution: Embrace automation and invest in robust RCM software that minimizes manual entry and automates error-checking.
5.4 Poor Communication with Payers
Pitfall: Misunderstandings and miscommunications with insurance payers can result in delayed reimbursements and claim denials. Solution: Establish clear lines of communication, maintain updated contact information for payer representatives, and promptly address any discrepancies in claim submissions.
6. The Future of Medical Billing Audits and Compliance
The healthcare industry is evolving, and so are billing practices:
- AI and Machine Learning: Emerging technologies are revolutionizing the billing process by automating claims submission, detecting errors in real time, and predicting potential denials before they occur.
- Blockchain for Security: Blockchain technology offers promising solutions for secure, transparent, and immutable records, which could further enhance billing accuracy and compliance.
- Enhanced Data Analytics: Advanced analytics tools provide deeper insights into billing performance, helping practices identify trends, improve cash flow, and optimize revenue cycles continuously.
By staying ahead of these technological trends, medical practices can not only improve their audit readiness but also ensure long-term compliance and financial stability.
7. Final Thoughts: Ensuring a Smooth Billing ProcessHandling medical billing audits effectively is a continuous process that requires a commitment to accuracy, compliance, and ongoing improvement. By preparing thoroughly for audits, responding promptly to auditor requests, and implementing corrective actions, healthcare practices can safeguard their revenue and maintain robust compliance with industry regulations.
Key Takeaways:
- Accurate Documentation: Ensure every service is fully documented and supported.
- Regular Training: Keep your billing and coding staff up-to-date with the latest practices.
- Embrace Technology: Automate where possible to reduce manual errors.
- Continuous Improvement: Use audit findings as a stepping stone for process enhancements.
- Proactive Communication: Maintain clear, ongoing communication with insurers and payers.
By integrating these best practices into your daily operations, your practice can reduce the risk of costly errors, speed up insurance reimbursements, and ultimately achieve a healthier cash flow.
How ClinicBillingHelp.com Can Assist You
At ClinicBillingHelp.com, our mission is to empower healthcare providers with the latest insights and practical strategies to optimize their revenue cycle management. Our comprehensive resources, expert guides, and industry updates are designed to help you navigate the complexities of medical billing audits and compliance. Whether you’re a small private practice or a large multi-specialty clinic, our content is tailored to provide actionable advice that can enhance your billing accuracy and financial stability.
Explore our collection of articles, checklists, and video tutorials to learn more about:
- Effective audit preparation techniques
- The latest regulatory changes in medical billing
- Best practices for integrating advanced RCM software into your workflow
Stay informed and up-to-date with ClinicBillingHelp.com, and transform your billing processes to maximize revenue and ensure compliance.
Conclusion
Medical billing audits are an inevitable part of managing a healthcare practice, but with the right strategies, they can be navigated smoothly. By investing in proper documentation, continuous staff training, automation, and proactive communication, you can minimize errors and maintain robust compliance. The future of medical billing lies in embracing innovative technologies such as AI and blockchain, which promise to further streamline the audit process and secure your practice’s financial health.
Implementing the strategies outlined in this guide will not only help you handle audits more effectively but also improve your overall revenue cycle management. With improved billing accuracy and reduced claim denials, your practice can enjoy faster insurance reimbursements and better cash flow, ensuring that you can focus on what matters most: providing exceptional patient care.
For more in-depth insights and expert guidance on optimizing your medical billing processes, visit ClinicBillingHelp.com. Our resources are dedicated to helping healthcare providers like you achieve compliance, reduce audit risks, and maximize revenue. Start exploring today and take the first step toward a more efficient, compliant, and profitable billing operation.