Introduction
If you’ve ever waited days—or even weeks—for a specialty drug approval due to prior authorization (PA), you’re not alone. For providers, payers, and especially patients, prior authorization has long been the bottleneck of specialty medication access. But that may soon change.
Enter Real-Time Benefit Tools (RTBTs)—technology-driven solutions that promise to slash delays, reduce administrative burden, and potentially offer instant prior authorization. Are we truly on the brink of real-time drug approvals? Or is this another tech promise that falls short in practice?
In this article, we’ll explore how RTBTs work, their impact on specialty drugs, payer adoption trends, and the evolving landscape of prior authorization in a post-digital era.
Understanding the Problem: Why Prior Authorization Has Become a Barrier
Prior authorization is a cost-control strategy used by health plans to ensure that certain drugs or procedures are medically necessary. While it helps prevent inappropriate prescribing and manages pharmacy spend, the process is often:
- Cumbersome: Involves faxes, phone calls, or portal logins.
- Opaque: Providers often don’t know what’s covered or how long it will take.
- Delaying Treatment: For critical specialty drugs, time-sensitive approvals can mean delayed care, worsening symptoms, or avoidable hospitalizations.
The situation becomes even more complex with specialty drugs, which are typically high-cost, require strict clinical criteria, and involve specialty pharmacies.
What Are Real-Time Benefit Tools (RTBTs)?
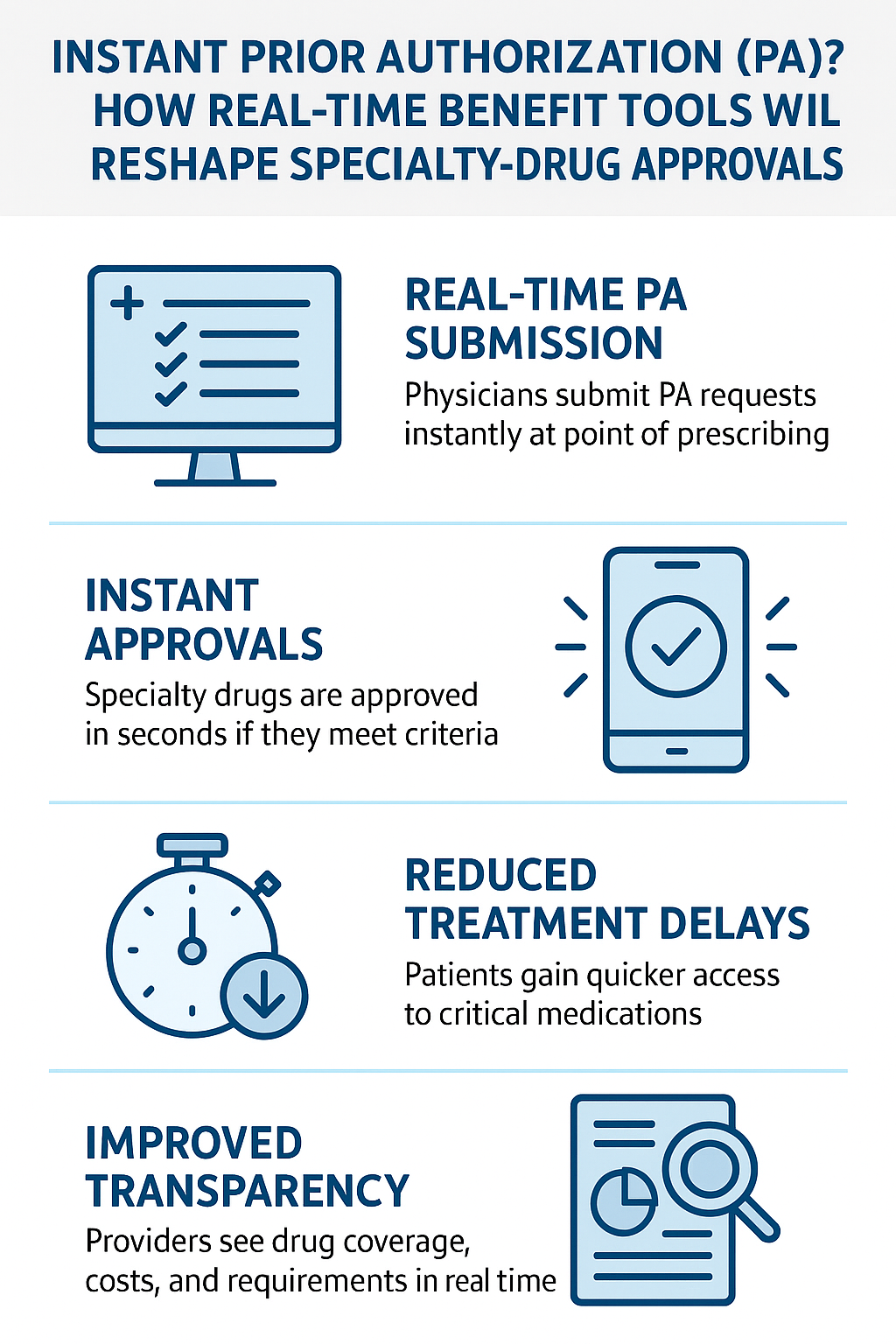
RTBTs are electronic solutions embedded within the provider’s EHR or e-prescribing system. They enable physicians to see:
- Drug coverage details
- Patient-specific copay or out-of-pocket costs
- Step therapy or formulary alternatives
- Prior authorization requirements—in real time
Some RTBTs even integrate electronic prior authorization (ePA), allowing providers to submit and receive PA decisions instantly, without leaving the workflow.
This is what positions RTBTs as a game-changer for specialty-drug approvals.
The Rise of Real-Time Drug Authorization for Specialty Medications
Until recently, real-time pharmacy benefit checks were limited to common medications. Specialty drugs—due to their complexity and multiple PA criteria—lagged behind.
However, next-gen RTBT platforms are now integrating clinical decision logic and payer-specific criteria to enable:
- Real-time PA submission from the point of prescribing
- Instant approvals for cases that meet all criteria
- Conditional approvals or streamlined denial with explanations
This evolution is pushing the boundaries of what “real-time authorization” means, especially for biologics, oncology drugs, and precision therapies.
How RTBTs Will Reshape the Specialty Drug Approval Ecosystem
-
Faster Time to Therapy
With real-time PA, patients may start treatment within hours rather than days or weeks. This is particularly vital in oncology, immunology, and rare disease treatments where time-sensitive interventions matter.
-
Fewer Abandonment Rates
One major reason patients abandon specialty medications is the wait time or cost uncertainty. RTBTs surface cost and PA status at the point of prescribing, leading to more informed—and actionable—decisions.
-
Provider Efficiency
Physicians no longer need to navigate separate portals or wait on faxed forms. Real-time visibility into approval pathways directly within the EHR reduces frustration and boosts efficiency.
-
Better Payer Control
RTBTs allow payers to dynamically enforce criteria without relying on retroactive review. They can guide providers toward preferred drugs and therapies in a seamless, transparent manner.
Is “Instant Prior Authorization” Truly Instant? The Limits of Real-Time Approvals
Despite the promise, it’s important to temper expectations. Not every specialty drug approval can or will be instant.
Reasons include:
- Complex Clinical Criteria: Some drugs require documentation that’s not immediately available in the EHR.
- Step Therapy Requirements: Payers may mandate failure of other therapies before approval.
- Manual Review: High-cost treatments often require human oversight or peer review.
Still, RTBTs can flag these requirements up front, eliminating guesswork and unnecessary submissions.
Adoption and Regulation: What’s Fueling the Growth of RTBTs?
-
CMS Mandates and Interoperability Initiatives
The Centers for Medicare & Medicaid Services (CMS) has been instrumental in pushing for RTBT integration across Medicare Part D plans. Under recent rules, Part D sponsors must offer prescribers access to real-time benefit information through a compliant tool.
This regulatory push is expanding RTBT availability across payers and platforms.
-
Integration with EHR Vendors
Major EHR systems like Epic, Cerner, and Athenahealth are increasingly embedding RTBTs into their e-prescribing modules, making it easier for providers to adopt without extra logins or tools.
-
Industry Collaborations
Tech giants, PBMs, payers, and specialty pharmacies are joining forces to create standardized APIs and platforms, enabling broader data exchange and interoperability.
Key Stakeholders in the Real-Time Authorization Movement
- Payers: Seeking better control and cost management while reducing provider abrasion.
- Providers: Wanting fewer administrative steps and faster answers for patients.
- Patients: Needing clarity and immediacy for costly, life-altering medications.
- Pharmacies: Coordinating with prescribers and plans to align on coverage and fulfillment timelines.
Successful RTBT adoption requires cooperation across this entire ecosystem.
Challenges Ahead: Where the Model Still Falls Short
-
Data Gaps Between Payers and Providers
Not all payers expose complete benefit data in real time. Inconsistent or incomplete datasets can lead to erroneous assumptions about PA requirements.
-
Lack of Standardization
RTBT platforms vary in functionality. Some only show pricing; others offer complete ePA. Without uniform expectations, provider trust may lag.
-
Specialty Pharmacy Integration
Even if a drug is approved instantly, the pharmacy fulfillment process (especially for white bagging or drop-shipped meds) can still introduce delays. End-to-end connectivity is key.
What Real-Time Prior Authorization Means for Revenue Cycle and Patient Access Teams
For hospital systems, infusion centers, and specialty clinics, real-time PA is not just a clinical win—it’s a revenue cycle accelerator.
- Quicker approvals reduce denied claims and rework.
- Patient access teams can verify benefits, coordinate refills, and track authorizations with greater clarity.
- Fewer treatment delays improve satisfaction scores and outcomes—critical for value-based care models.
RTBTs can also support automated appeals if a denial is issued, further improving turnaround.
Future Outlook: Will All Specialty Drugs Be Approved in Real Time?
While instant authorization may not be possible for every case, the trend is clear: the future of specialty medication access is digital, automated, and real-time-informed.
Expect to see:
- Broader integration of AI-based criteria matching for real-time approvals
- Greater payer participation in RTBT networks
- Expansion beyond pharmacy to include medical benefit drugs
- Growing adoption of FHIR-based APIs for true interoperability
FAQs About Real-Time Benefit Tools and Instant PA
-
Q: Do real-time benefit tools eliminate the need for prior authorization?
No. They surface the need for PA upfront and may help automate the submission, but the clinical criteria still apply.
-
Q: Are RTBTs available for all providers?
Not yet. Availability depends on EHR system integration and whether the provider’s payers participate in RTBT networks.
-
Q: Can patients use RTBTs to see their own drug costs?
Some tools are consumer-facing, but most are designed for providers during the prescribing process.
-
Q: Will RTBTs apply to medical benefit drugs like infusions?
This is an emerging area. Some vendors are beginning to extend real-time logic to medical benefit claims, but it’s still early.
Conclusion: A Turning Point in Specialty Drug Authorization
What once took days or weeks may soon take minutes—or seconds. Real-time benefit tools are shifting the landscape of specialty drug access from fragmented and frustrating to connected and streamlined.
While we may not be at universal “instant prior authorization” just yet, we’re closer than ever to real-time, criteria-based approvals that empower physicians and improve patient care.
For stakeholders in the healthcare system, now is the time to embrace, integrate, and refine RTBT capabilities—because the future of specialty care depends on it.




