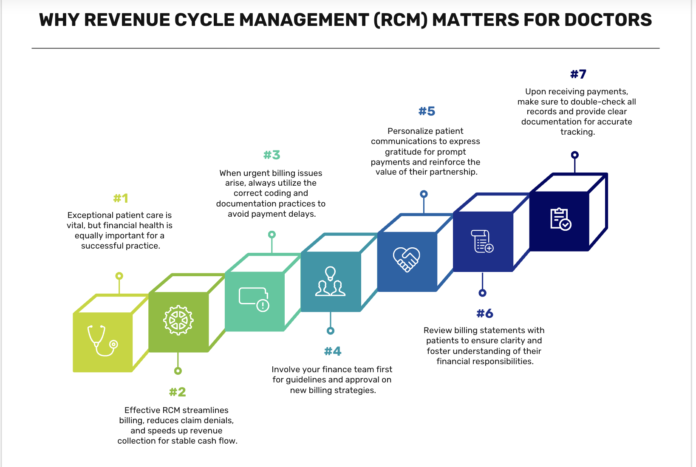
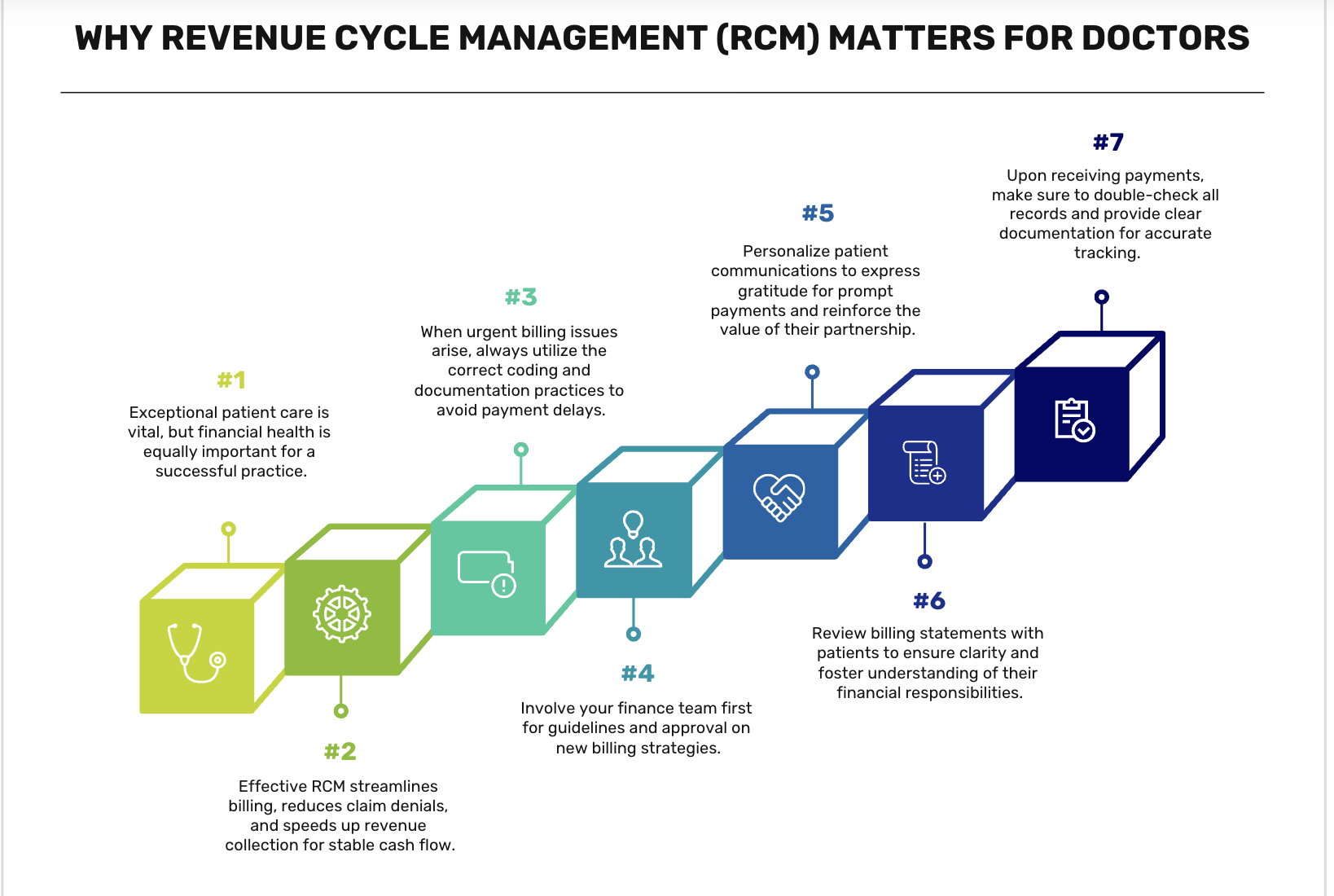
Introduction: Why Revenue Cycle Management (RCM) Matters for Doctors
A successful medical practice is not just about delivering high-quality patient care—it’s also about ensuring financial stability. Revenue Cycle Management (RCM) plays a critical role in the healthcare industry by helping doctors and clinics streamline billing, reduce denials, and accelerate payments from both insurers and patients.
Understanding the 7 stages of RCM allows healthcare providers to improve cash flow, reduce administrative burden, and minimize revenue losses.
This guide will break down each stage of RCM, explaining how doctors and medical staff can optimize these processes to maintain a healthy revenue stream.
1. Patient Registration & Insurance Verification
The first stage of RCM begins when a patient schedules an appointment and their demographic and insurance information is collected.
Key Steps in Patient Registration:
- Gather personal details (name, DOB, address, contact info).
- Verify insurance eligibility and coverage details.
- Check for deductibles, co-pays, and prior authorizations.
- Obtain necessary referrals if required by the insurance provider.
Why This Matters:
Reduces claim denials due to incorrect insurance information. Ensures faster payments by confirming coverage before services are provided. Avoids billing disputes by informing patients of their financial responsibility upfront.
How to Optimize:
- Use real-time insurance verification tools to check patient eligibility instantly.
- Train front-desk staff to collect accurate and complete patient details.
2. Medical Coding & Charge Capture
Once a patient receives medical care, services must be accurately documented and coded for billing.
Key Steps in Medical Coding & Charge Capture:
- Convert medical diagnoses and procedures into ICD-10, CPT, and HCPCS codes.
- Ensure codes match the level of service provided to avoid undercoding or overcoding.
- Use electronic charge capture to eliminate manual errors.
Why This Matters:
Reduces claim rejections by ensuring proper coding. Maximizes reimbursement rates by capturing all billable services. Improves compliance with payer regulations.
How to Optimize:
- Invest in AI-powered medical coding software to reduce manual errors.
- Train medical coders and billing staff to stay updated on coding changes.
3. Claims Submission & Processing
Once medical codes are assigned, claims must be submitted to insurance companies for reimbursement.
Key Steps in Claims Submission:
- Ensure all required patient and provider details are correct.
- Submit claims electronically via EDI (Electronic Data Interchange).
- Track claim status to identify rejections early.
Why This Matters:
Avoids payment delays by ensuring clean claims. Reduces claim rejections due to missing or incorrect data. Improves revenue flow by accelerating insurance reimbursements.
How to Optimize:
- Use automated claims submission tools to speed up the process.
- Implement claim scrubbing software to detect errors before submission.
4. Claims Adjudication & Denial Management
After submission, insurance companies review claims to determine reimbursement eligibility.
Key Steps in Claims Adjudication:
- The payer reviews patient eligibility, coding accuracy, and policy coverage.
- If the claim is approved, payment is processed.
- If denied, the payer provides a denial reason code.
Why This Matters:
Claim denials result in revenue losses if not managed properly. Identifying patterns in denials helps improve future claim approvals. Faster appeals lead to quicker payments.
How to Optimize:
- Track and analyze denial patterns to reduce future errors.
- Establish a structured appeal process for denied claims.
- Set up automated alerts for claim denials to take quick action.
5. Payment Posting & Reconciliation
Once claims are approved, payments must be posted and reconciled with patient accounts.
Key Steps in Payment Posting:
- Post payer reimbursements and patient payments into the system.
- Reconcile payments with billed amounts to identify discrepancies.
- Flag underpayments or overpayments for resolution.
Why This Matters:
Identifies unpaid claims quickly to take corrective action. Ensures correct patient balances before sending bills. Prevents financial discrepancies that affect revenue tracking.
How to Optimize:
- Automate payment posting to match EOBs (Explanation of Benefits).
- Reconcile payments weekly to avoid billing inconsistencies.
6. Patient Billing & Collections
If a balance remains after insurance payments, patients must be billed for the remaining amount.
Key Steps in Patient Billing:
- Generate clear, itemized patient statements.
- Offer multiple payment options (credit card, online, installment plans).
- Send automated payment reminders to reduce overdue accounts.
Why This Matters:
Avoids revenue losses from unpaid patient balances. Enhances patient satisfaction with clear billing communication. Improves collection rates by offering easy payment methods.
How to Optimize:
- Implement online payment portals for seamless transactions.
- Offer discounts for early payments to incentivize collections.
7. Reporting & Performance Optimization
The final stage of RCM involves analyzing financial performance and optimizing revenue cycle workflows.
Key Steps in RCM Reporting:
- Track claim approval rates, denial reasons, and collection trends.
- Identify revenue leaks through data-driven insights.
- Optimize payer contract negotiations to maximize reimbursements.
Why This Matters:
Helps detect inefficiencies in the billing cycle. Improves financial forecasting for better cash flow management. Enhances decision-making with real-time analytics.
How to Optimize:
- Use RCM dashboards to monitor key performance metrics.
- Conduct monthly revenue cycle audits to identify improvement areas.
Final Thoughts: Why Every Doctor Should Optimize RCM
An efficient Revenue Cycle Management (RCM) process is essential for doctors and healthcare providers to reduce revenue losses, improve cash flow, and enhance patient satisfaction.
By optimizing insurance verification, claims submission, denial management, and patient billing, clinics can ensure steady revenue generation.
Implementing automation, AI-driven coding tools, and real-time analytics can significantly boost RCM efficiency.
At ClinicBillingHelp.com, we provide expert guides, billing best practices, and industry insights to help doctors navigate the complexities of RCM and improve their practice’s financial health.
Looking for more RCM insights?
Explore expert articles and resources at ClinicBillingHelp.com.