Credentialing is often seen as a tedious necessity—critical for patient safety and payer compliance, yet plagued by delays, redundancies, and paperwork overload. For health plans and provider networks accredited by the National Committee for Quality Assurance (NCQA), every step of the credentialing process is governed by precise standards. But does compliant always mean slow?
Not necessarily.
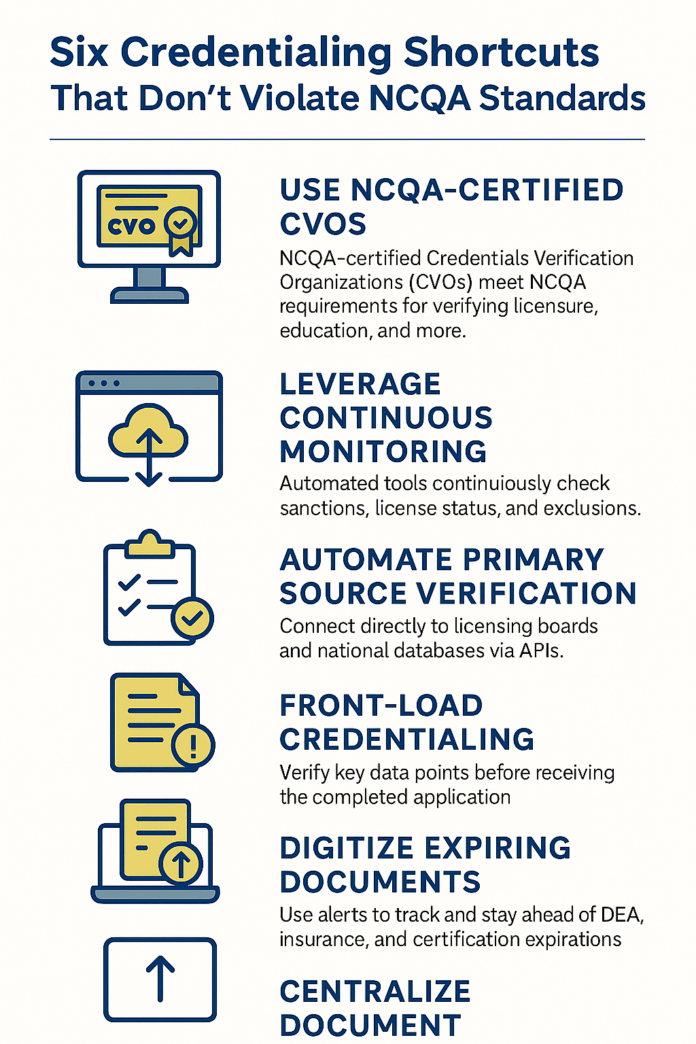
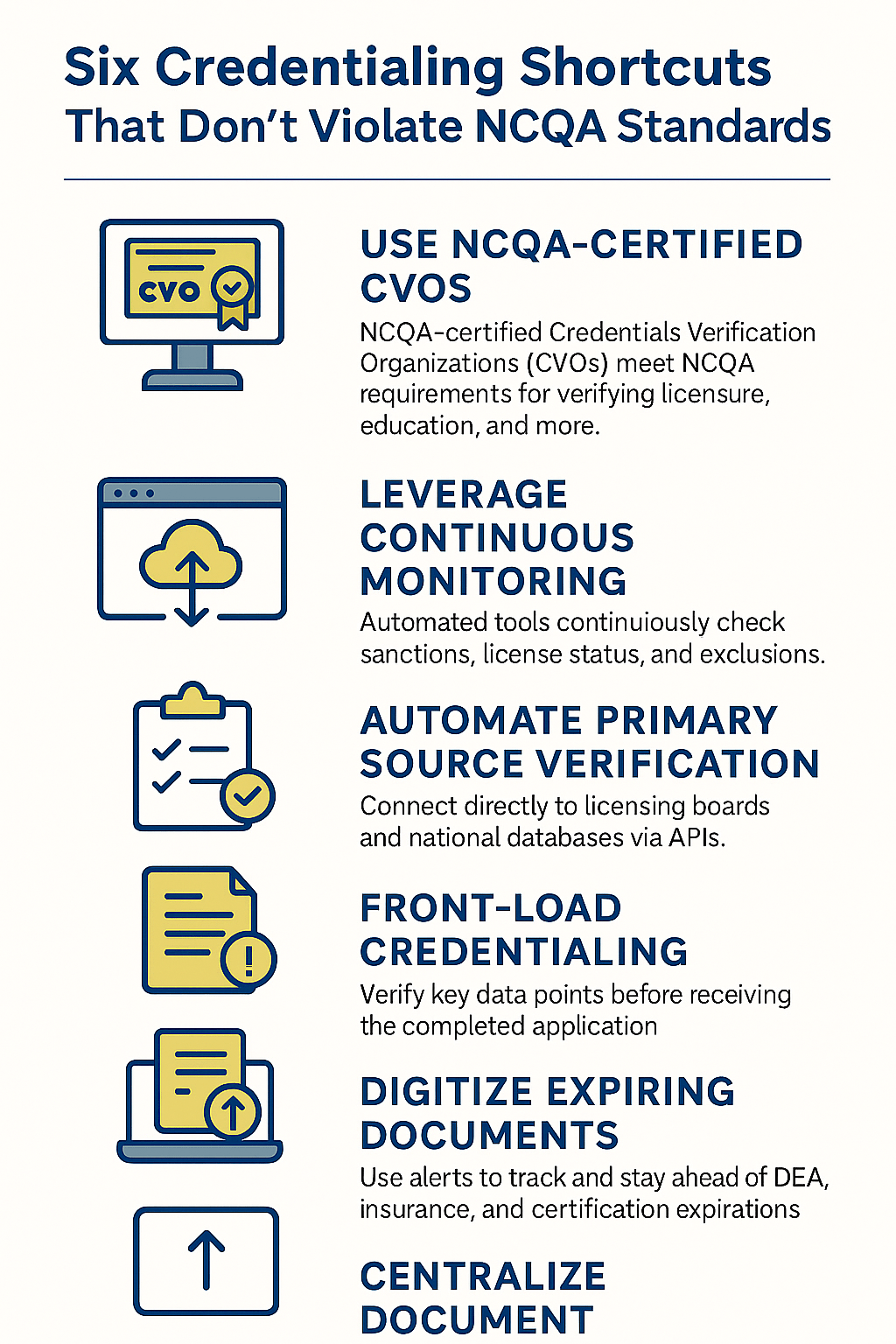
There are legitimate shortcuts that don’t cut corners—but instead optimize workflows, use approved data sources, and improve turnaround time without compromising NCQA standards. In this article, we uncover six credentialing shortcuts that speed things up while remaining 100% compliant with NCQA’s credentialing requirements.
Understanding the NCQA Credentialing Framework
Before diving into the shortcuts, it’s important to clarify the NCQA’s position: Speed is not the enemy—non-compliance is.
NCQA’s credentialing standards (CR 1–CR 7) focus on:
- Timely verification of credentials
- Use of primary source verification (PSV)
- Regular credentialing every three years
- Peer review and sanctions checks
- Delegation and oversight
What they don’t prohibit is innovation—if you can prove verification, follow required timelines, and maintain documentation, you’re in the clear.
Shortcut 1: Use NCQA-Certified Credentials Verification Organizations (CVOs)
Time saved: 30–50%
NCQA-compliant? Yes – per CR 1 and CR 6
If your in-house credentialing team is overwhelmed or lacks robust systems for primary source verification, partnering with a CVO certified by NCQA is one of the safest shortcuts. These vendors are pre-approved to conduct verifications like licensure, DEA registration, education, and board certification.
Why it works:
- Eliminates manual verification tasks
- Reduces error-prone back-and-forth
- Ensures all verifications meet NCQA standards and timeframes
Pro tip: Always validate the CVO’s NCQA certification status and include it in your credentialing file as part of the delegation oversight process.
Shortcut 2: Leverage Continuous Monitoring for Sanctions and License Status
Time saved: Eliminates the need for batch monthly checks
NCQA-compliant? Yes – aligns with CR 6 and CR 7
Traditional credentialing requires checking for Medicare/Medicaid sanctions, license status, and exclusions at specific intervals. However, real-time monitoring tools now automate this, providing continuous updates via integrated alerts.
Why it works:
- Detects changes faster than batch checks
- Creates automatic documentation trails
- Supports proactive risk management for providers with red flags
Caveat: Be sure to validate that the data sources are approved by NCQA, such as FSMB, OIG, NPDB, and state licensing boards.
Shortcut 3: Automate Primary Source Verification via APIs
Time saved: Reduces PSV task time from days to minutes
NCQA-compliant? Yes – when verified against required sources
Modern credentialing systems allow you to connect directly to licensing boards and national databases via secure APIs. Instead of downloading PDFs or making manual queries, the system pulls real-time verification data instantly.
Why it works:
- Improves audit readiness with digital logs
- Ensures verification is timestamped and source-tracked
- Reduces clerical delays without skipping any required step
APIs can be configured to automatically recheck if a source is temporarily unavailable, ensuring compliance without delays.
Shortcut 4: Front-Load Credentialing with Pre-App Verification
Time saved: Shortens turnaround after provider submission
NCQA-compliant? Yes – when documentation is retained and within the 180-day validity period
Most credentialing teams wait until a provider completes their application before beginning verifications. But you can begin verifying key data points (like licenses, DEA, and sanctions) before the application is complete—as long as the information is current within the NCQA’s 180-day window.
Why it works:
- Speeds up the “clock start” once the application is complete
- Prevents bottlenecks due to predictable issues like expired licenses
- Allows more focused follow-up on application gaps
This shortcut is particularly effective when onboarding high volumes of providers for urgent expansions or payer panels.
Shortcut 5: Digitize and Auto-Track Expiring Documents
Time saved: Reduces delays from chasing outdated certifications
NCQA-compliant? Yes – CR 2 requires current documentation, not paper-based storage
Credentialing backlogs often stem from expired DEA certificates, lapsed insurance, or outdated board certifications. By using credentialing software with built-in expiration alerts, you can notify providers well in advance, reducing the time you spend chasing renewals.
Why it works:
- Ensures documents remain valid within NCQA’s 180-day window
- Builds a proactive renewal pipeline
- Supports auto-reminders for recredentialing deadlines
This shortcut also helps during audits by showing automated proof of outreach and timeline compliance.
Shortcut 6: Centralize Document Submission Through Provider Portals
Time saved: Cuts document collection time by up to 60%
NCQA-compliant? Yes – as long as secure access and documentation standards are met
Rather than relying on email chains or fragmented communication, provider portals allow physicians to upload documents, track progress, and receive alerts in one place. Some credentialing systems integrate with CAQH to auto-populate common fields, reducing redundancy.
Why it works:
- Reduces administrative friction
- Improves accuracy and completeness
- Provides an audit trail with submission timestamps
Ensure the portal meets HIPAA and NCQA standards for document handling, especially when dealing with sensitive information like malpractice history.
Common Myths About Credentialing Speed vs. NCQA Compliance
Let’s bust a few myths that keep organizations from optimizing their process:
- Myth: You can’t use third-party data sources.
- Truth: NCQA allows certified CVOs and approved electronic data sources.
- Myth: Everything must be done manually to be compliant.
- Truth: Automation is fine—if the source is valid and documentation is retained.
- Myth: Credentialing faster means cutting corners.
- Truth: Cutting waste is not the same as cutting corners. Efficiency can enhance—not erode—compliance.
Benefits of Implementing These Shortcuts
Aside from staying compliant, these shortcuts deliver:
- Faster provider onboarding: Essential for large practices, hospital systems, and expanding payor networks
- Reduced administrative burden: Your credentialing staff can focus on critical issues rather than paperwork
- Improved audit readiness: Digital records simplify responses to NCQA, URAC, or state audits
- Better provider satisfaction: Timely credentialing reduces frustration and enhances reputation
FAQs: Credentialing Shortcuts and NCQA Standards
Q: What is the NCQA’s credentialing timeframe for verifications?
Verifications must be current within 180 calendar days prior to the credentialing committee decision date.
Q: Can I credential someone faster than 30 days and still be compliant?
Yes, speed is not the issue—accuracy and completeness are. If all verifications are completed correctly, even a 10-day file is compliant.
Q: Can expired documents delay credentialing?
Absolutely. That’s why auto-tracking expirations and alerting providers ahead of time is a key shortcut.
Q: Are e-signatures acceptable for provider attestations?
Yes, if they are secure and traceable. NCQA accepts electronic signatures with proper audit trails.
Conclusion: Credentialing Smarter, Not Slower
Credentialing doesn’t have to be the slowest step in your revenue cycle. By implementing these six shortcuts, organizations can streamline onboarding, reduce errors, and meet compliance with confidence. The goal is not to sidestep NCQA—it’s to stay in alignment while moving faster and more efficiently.
Speed and compliance are not mutually exclusive. In fact, when done right, they go hand in hand.