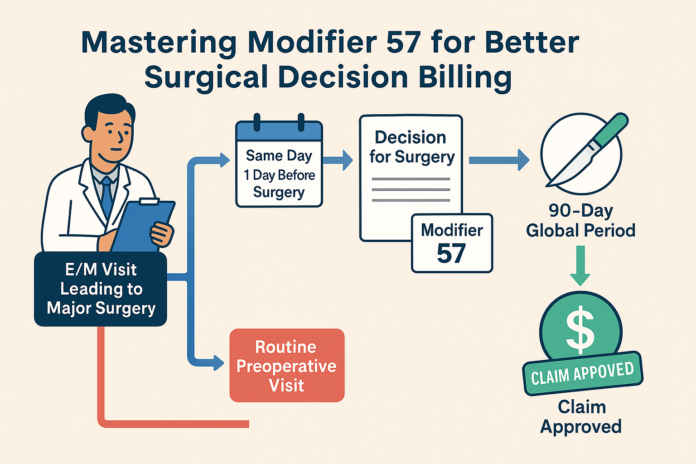
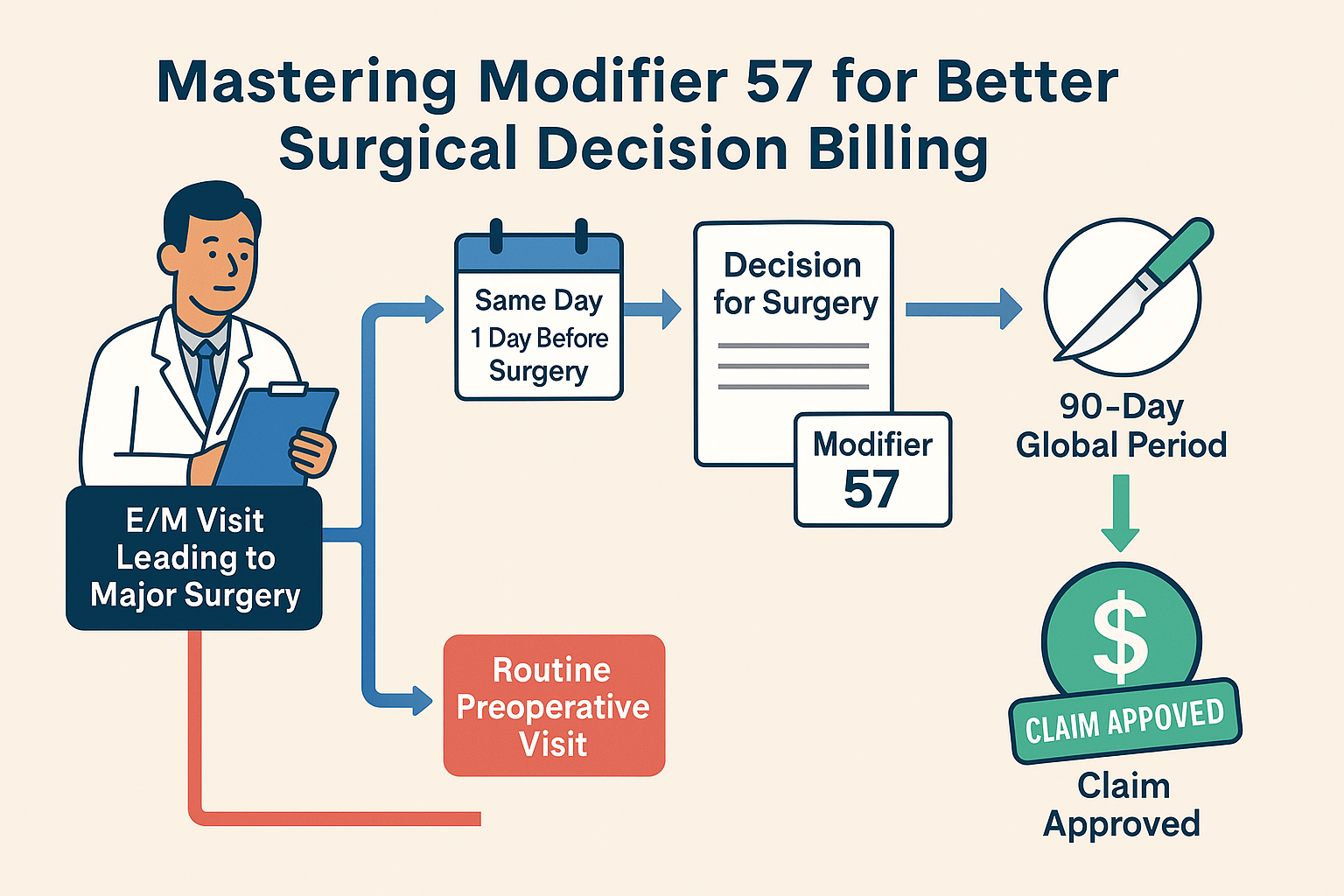
Modifier 57 is a key player in surgical billing, yet it often confuses healthcare professionals striving to optimize revenue. Attaching this modifier informs payers that an Evaluation and Management (E/M) service resulted in the decision to perform a major surgical procedure—typically one with a 90-day global period. In this comprehensive guide, we’ll break down everything from documentation best practices to real-world scenarios. Our goal is to ensure you can accurately use Modifier 57, stay aligned with payer rules, and safeguard your revenue.
By the end of this article, you will:
- Understand the fundamentals of Modifier 57 and why it’s crucial.
- Know how timing, documentation, and payer-specific policies influence reimbursement.
- Learn how to avoid claim denials by distinguishing between a standard preoperative visit and the genuine decision for surgery.
- Gain confidence in navigating common pitfalls, so you can maintain compliance and capture legitimate earnings.
1. What Is Modifier 57?
Modifier 57 is a Current Procedural Terminology (CPT) modifier that specifically indicates an E/M service resulted in the initial decision to perform a major surgical procedure. A “major surgery” typically has a global period of 90 days, although in some cases, 10-day or other lengths may apply if the procedure is considered extensive.
Why Does Modifier 57 Matter?
- Reimbursement Integrity: If a significant surgical procedure is performed, insurance payers consider the preoperative work bundled into the global surgical package—unless it’s separately distinguishable as the decision-making visit.
- Avoiding Denials: Without Modifier 57 appended to the E/M code, many payers might view the visit as part of the normal preoperative workup and deny separate payment.
- Compliance: Using Modifier 57 improperly can lead to audits and potential paybacks. Understanding when it’s appropriate ensures compliance with payer guidelines.
In essence, Modifier 57 says: “This evaluation led to the decision for a major operation, so it merits separate payment distinct from the surgery’s global package.”
2. Understanding Major Surgery and Global Periods
Defining Major Surgery
- Global Period: Major surgeries typically carry a 90-day global period. During this period, routine postoperative visits and related services are bundled.
- High Complexity: Major surgeries are often considered high complexity in terms of risk, resources, and potential complications.
What Are Global Periods?
A global period (sometimes called a “global surgical package”) bundles certain preoperative, intraoperative, and postoperative services into a single payment. For most major surgeries, Medicare and many private payers impose a 90-day global period. Minor procedures might have 0-day or 10-day global periods.
- Zero-Day or 10-Day Global: Typically for minor procedures. Modifier 57 is not generally used here.
- 90-Day Global: Common for procedures like joint replacements, open abdominal surgeries, or significant orthopedic interventions.
Key Point: Modifier 57 only applies for major procedures—usually those with a 90-day global. For minor surgeries, you might consider other modifiers (e.g., Modifier 25 for significant, separately identifiable E/M on the same day of a minor procedure).
3. When to Use Modifier 57
1. E/M Service Leading to Major Surgery
If, after an evaluation, the provider concludes that a major surgical procedure is medically necessary, you should attach Modifier 57 to the E/M code. This indicates the service is separately payable because it required significant decision-making.
2. Same or Next Day Decision for Surgery
Often, the decision and the procedure happen on the same day or the day immediately preceding. Modifier 57 clarifies that the E/M service that day (or the day before) was the critical decision point.
3. Complex Conditions
When a patient presents with an emergent or life-threatening condition (e.g., acute appendicitis) and the physician decides to operate, use Modifier 57 on the E/M service that made that decision clear.
4. Key Timing Considerations
Same Day vs. Different Day
Many times, the patient is evaluated on the same day they need the surgery—especially in urgent or emergent cases. In such scenarios:
- E/M code for the Decision: Append Modifier 57.
- Surgery code: Report without Modifier 57 (since the procedure code stands alone for the surgery).
If the decision happens the day before surgery, you’d still append Modifier 57 to the E/M code from that day.
Avoiding Double Billing
Be mindful if multiple visits are billed in close proximity to the surgery. Ensure you aren’t mistakenly appending Modifier 57 to all. It should only go on the visit where the surgeon determined surgery was needed.
Late or Complex Diagnoses
In certain complex conditions—like discovering an unexpected malignancy—surgeons may need an additional visit to discuss a change in surgical plan or the need for a more extensive procedure. If the decision to switch from a minor to a major procedure is made at this second visit, that E/M service may warrant Modifier 57 if it changes the scope of surgery.
5. Essential Documentation Practices
Establish Medical Necessity
Payers pay extra attention to surgeries with significant expenses. To justify separate payment for an E/M service, document:
- Chief Complaint: What issue prompted the E/M service?
- History of Present Illness (HPI): Detail the events leading to the condition requiring surgery.
- Physical Examination: Focus on the findings that led you to conclude surgery is necessary.
- Assessment/Plan: Clearly state the rationale for surgery, ideally referencing the potential risks, benefits, and alternatives discussed with the patient.
Clearly Note the “Decision for Surgery”
In the assessment and plan section, write something like:
“Patient’s acute abdominal pain, elevated WBC count, and imaging studies are consistent with acute appendicitis. Decision made to proceed with urgent appendectomy.”
This explicit statement helps coders and auditors see the direct link between the E/M service and the conclusion that surgery is needed.
Use Specific Diagnosis Codes
For instance, if you discovered an abdominal mass suspicious for malignancy, ensure your ICD code is precise (e.g., “Neoplasm of colon, malignant” rather than a generic “Abdominal pain”). The clarity in diagnosis coding supports the necessity and complexity of the decision.
6. Distinguishing a Preoperative Visit from the Decision for Surgery
One of the biggest pitfalls is incorrectly claiming an E/M service that’s purely “preoperative clearance” or “routine preop exam” as a decision for surgery. Routine preoperative exams typically fall under the surgical package—especially if the surgery was already planned.
Preoperative Visit (Usually Bundled)
- Occurs after the decision has already been made.
- Involves standard evaluations such as lab reviews, EKG, or other risk assessments.
- Routine instructions on NPO (nothing by mouth) guidelines, scheduling details, and typical surgical prep.
Decision for Surgery Visit (Modifier 57 Applicable)
- This is where the provider is still determining whether a major surgery is indicated.
- Often includes substantial new diagnostic workups, additional imaging, or lab tests that confirm or rule out the need for an operation.
- Includes a formal recommendation: “Yes, surgery is now the recommended course of treatment.”
Tip: When auditing your documentation, ask, “Was the surgery already decided prior to this visit?” If yes, it’s likely a preop visit (bundled). If not, it may be a legitimate scenario for Modifier 57.
7. Examples & Scenarios
Scenario A: Urgent Gallbladder Surgery
- Patient Presentation: Severe right upper quadrant pain, fever, and positive ultrasound for gallstones.
- Analysis: The physician’s evaluation determined the patient has acute cholecystitis requiring immediate cholecystectomy.
- Coding: Bill an E/M service (e.g., 99284, 99285 if in the ED or 99213-99215 in the office) with Modifier 57. Then, separately bill for the cholecystectomy without Modifier 57.
Scenario B: Oncology Decision-Making
- Patient Presentation: A biopsy confirms a malignant breast lesion. During a subsequent E/M visit, the oncologist and surgeon confer and decide on a mastectomy.
- Analysis: Although there was a suspicion of a need for surgery earlier, the final definitive decision is made at this visit based on biopsy results.
- Coding: Append Modifier 57 to the E/M code from the date the final surgical plan is formed and documented.
Scenario C: Planned Surgery vs. Additional Decision
- Patient Presentation: The patient was already scheduled for a laparoscopic hernia repair. In reviewing preoperative labs, the surgeon discovers an unrelated but urgent condition requiring a more invasive procedure.
- Analysis: If the existing surgery was already planned, you wouldn’t add Modifier 57 for that. But if the additional condition calls for a second major procedure—decided on at that visit—Modifier 57 may apply to that new decision.
- Coding: Bill E/M with Modifier 57 for the newly discovered major procedure only.
8. Common Mistakes and How to Avoid Them
-
Using Modifier 57 for Minor Procedures
- Mistake: Appending Modifier 57 for a procedure that has a 0- or 10-day global period.
- Fix: Use Modifier 25 instead if you have a significant, separately identifiable E/M service on the same day of a minor procedure.
-
Appending Modifier 57 to All E/M Visits Before Surgery
- Mistake: Attaching Modifier 57 simply because the patient is having surgery the next day, even if the decision was made weeks ago.
- Fix: Only append Modifier 57 to the visit where the decision was actually made.
-
Lack of Clear Documentation
- Mistake: The medical record doesn’t explicitly show the thought process or mention “decision for surgery.”
- Fix: Spell it out. Include phrases like “After reviewing findings, we decided that a total knee replacement is medically necessary.”
-
Confusing Preoperative Clearance with a Decision for Surgery
- Mistake: Using Modifier 57 for routine preop labs and instructions.
- Fix: Distinguish routine preop from actual decision-making. If the surgery was planned already, don’t use Modifier 57.
-
Not Checking Payer Policies
- Mistake: Assuming all payers handle Modifier 57 the same.
- Fix: Verify payer-specific guidelines. Some payers might require additional documentation or have specific forms.
9. Payer-Specific Rules and Variations
While Medicare guidelines are a reliable reference point, keep in mind:
- Private Payers: Some private insurers may have different interpretations or time windows (e.g., “Must attach Modifier 57 if the decision and surgery happen within 24 hours.”).
- Medicaid Plans: States can have variable rules. Always verify local regulations.
- Managed Care Organizations: HMOs or PPOs might require pre-authorization or additional proof that the decision was finalized at that encounter.
Tip: Maintain a payer matrix—an internal reference listing each major insurer’s stance on Modifier 57 usage, common denial reasons, and required documentation.
10. Strategies to Optimize Revenue and Avoid Denials
-
Educate Your Team
- Conduct periodic training sessions for physicians, coders, and billing staff.
- Provide quick reference guides that define major surgery and detail when to use Modifier 57 vs. other modifiers.
-
Implement a Documentation Checklist
Ensure each E/M note that leads to major surgery includes:
- Chief complaint.
- Relevant diagnostic findings.
- Clear statement: “Decision made to proceed with [surgery name].”
This evidence-based approach reduces the risk of payer audits.
-
Use Smart EHR Prompts
If your Electronic Health Record allows, set up an alert that asks:
“Was this visit the first time you decided on major surgery for this patient?”
This helps clinicians remember when to apply Modifier 57.
-
Regular Internal Audits
- Periodically review claims that used Modifier 57.
- Confirm each instance has robust documentation supporting a new decision for a major surgery.
-
Track Denials and Appeals
Maintain a log of denial reasons. If you notice repeated denials on Modifier 57 claims, investigate patterns such as insufficient documentation or incorrect CPT usage.
-
Stay Current on Coding Guidelines
Coding regulations can change. Subscribe to CMS updates, attend webinars, and network with specialty associations to remain informed.
11. Review: Key Takeaways
-
Modifier 57 Applies to Major Surgery Decisions
- It’s reserved for E/M visits where a physician concludes surgery is necessary for a condition requiring a global period (often 90 days).
-
Documentation Must Show the Decision
- Include clinical findings, diagnostic test results, and a statement that confirms you arrived at the decision for surgery during that visit.
-
Timing is Crucial
- Typically appended when the E/M service happens on the same or preceding day of surgery. Avoid confusion with routine preoperative visits.
-
Common Pitfalls
- Using Modifier 57 for minor procedures, unclear notes, or standard preop checks can invite denials and potential audits.
-
Payer Policies Vary
- Always confirm whether the payer has specific guidelines or additional requirements. Keep an updated reference for staff.
12. Conclusion
Modifier 57 is a powerful yet often misunderstood element in surgical billing. By clarifying that an E/M service led to a major surgery decision, healthcare providers can rightfully claim reimbursement for the cognitive labor and risk assessment that goes into planning surgery. Proper usage hinges on timely, detailed, and accurate documentation that unambiguously shows the turning point: “Yes, we must operate.”
Failing to master Modifier 57 can mean missing out on legitimate revenue or facing claim denials. On the other hand, consistent and appropriate application underscores your commitment to compliance, transparency, and robust revenue cycle management. Whether you’re working in a large hospital setting or a small private practice, understanding the nuances of Modifier 57 will help you maintain the financial health of your organization and preserve the trust of payers.
Remember these final pointers:
- Clearly document the clinical necessity and the final decision within the same E/M note.
- Use Modifier 57 only for major surgeries—specifically those with a 90-day global period.
- Continue to refine your processes and education efforts to keep your team aligned with the latest payer rules.
With the right knowledge and systems in place, you can confidently navigate Modifier 57, ensuring your services are paid for appropriately and your practice remains compliant. By differentiating true decision-making visits from routine preoperative assessments, you’ll elevate your billing accuracy, streamline your revenue cycle, and ultimately better serve your patients’ needs.